Quick Summary
Pazcare has simplified group health insurance by removing manual work, integrating with HR systems, and creating a uniform experience across insurers and TPAs.
Pazcare has simplified group health insurance by removing manual work, integrating with HR systems, and creating a uniform experience across insurers and TPAs.
Over the last six months, our product focus at Pazcare has been very clear:
Remove friction, reduce dependency on broken workflows, and deliver a truly uniform experience across group health insurance at scale.
This post is a summary of what we’ve shipped recently and why it matters for HR, finance teams, and employees.
Group health insurance today suffers from deep fragmentation:
The outcome is predictable:
Our work over the last six months has been about fixing this experience layer, not patching around it.
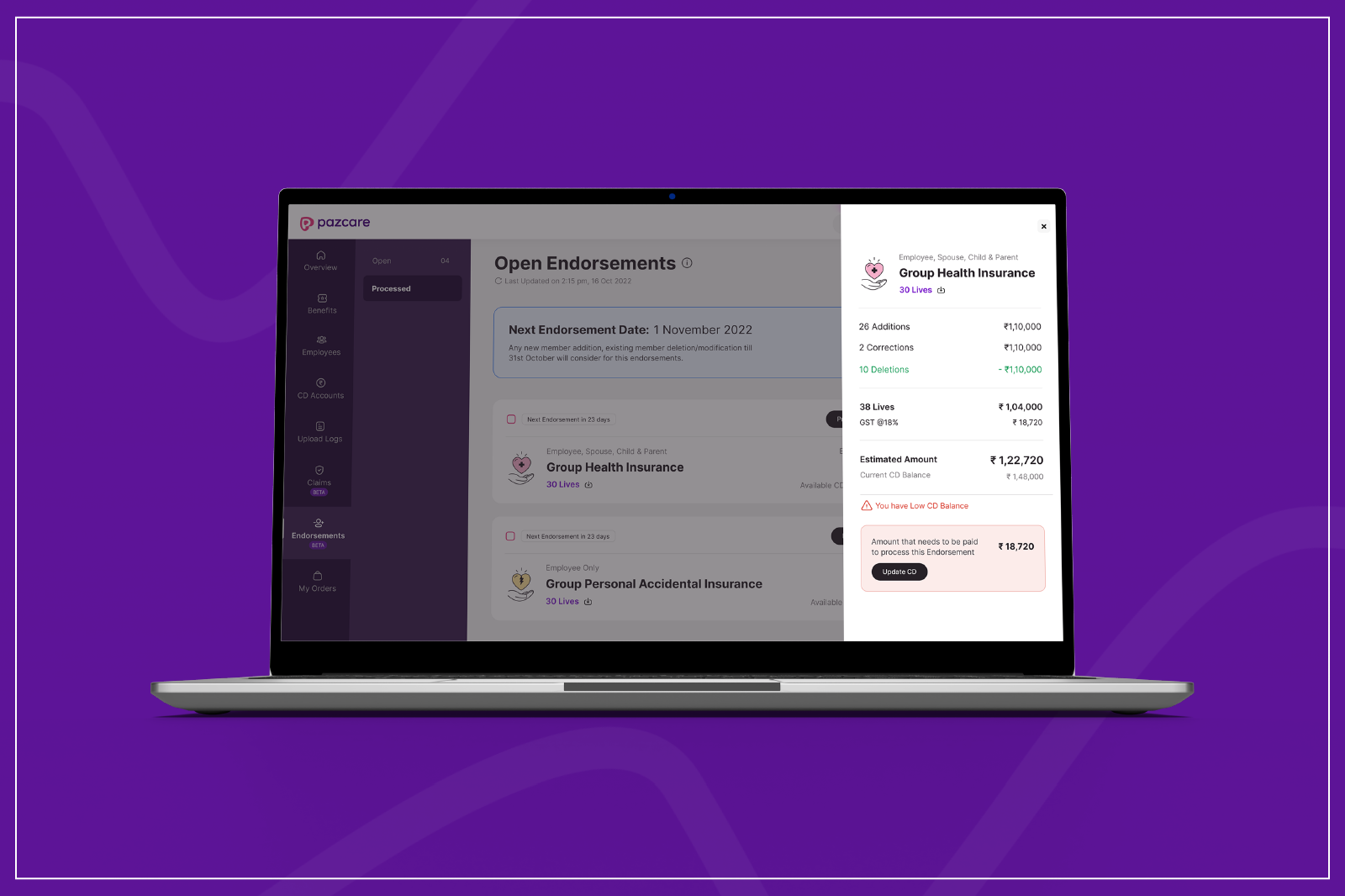
We launched several features to make insurance administration predictable and self-serve:
These changes significantly reduce back-and-forth between HR teams, the Pazcare team, insurers, and finance teams, eliminating dependency on manual follow-ups and fragmented communication.

Insurance workflows should move automatically with employee data—not require rework.
We built native integrations with leading HRMS platforms like Darwinbox, KekaHR, HROne and similar systems, enabling:
Claims are where experience breaks most often.
Our data showed that ~40% of claims get stuck due to queries.
Many of these queries are:
This leads to delays, confusion, and frustration—despite the claim being otherwise valid.
Instead of relying on insurer or TPA portals which often suffer from legacy UX and delayed updates, we built direct APIs with multiple insurers and TPAs.
This allows us to:
As a result, the experience no longer breaks simply because a different insurer or TPA is involved.
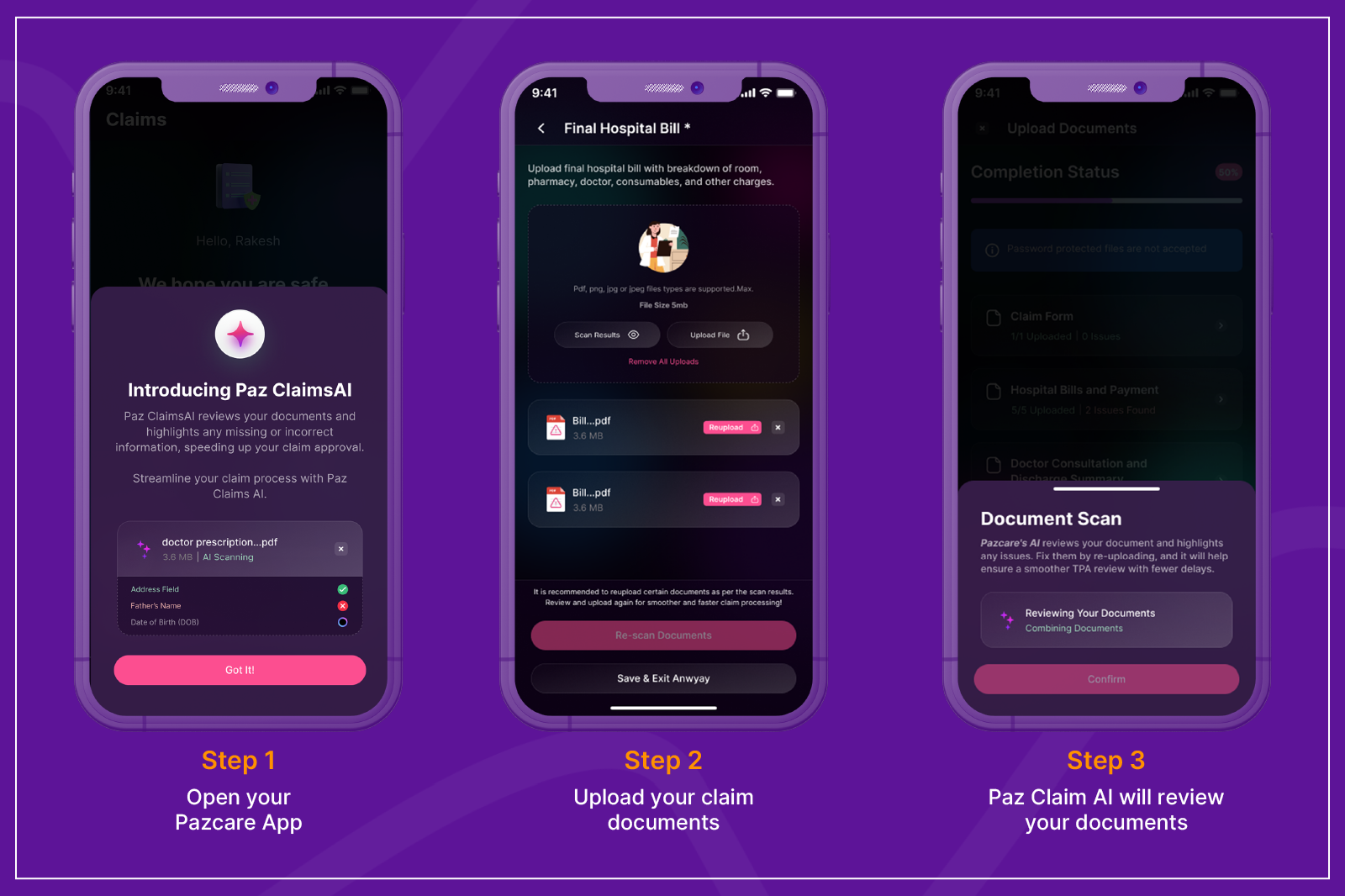

On top of API integrations, we introduced Claims AI to improve claim outcomes.
Claims AI helps by:
We are now progressing towards:
A key by-product of routing everything through our platform is visibility.
This benefits HR teams and employees alike, while also strengthening the overall ecosystem. The data enables us to advise clients on the best options based on real performance, and helps our insurer and TPA partners clearly understand where they stand against benchmarks especially in areas impacted by legacy UX and delayed updates.
We can now:
Where We’re Headed
Our core belief remains unchanged:
The last six months were about laying the foundation.
What comes next is deeper automation, faster resolution, and an even more invisible insurance experience.
More updates soon.

